Are You a Long Hauler?
The full spectrum and severity of COVID-19 symptoms continue to surface. For those who get infected with the SARS-CoV-2 virus, the symptoms can range from mild flu-like symptoms to severe infection resulting in acute respiratory distress syndrome, and hyperinflammation (cytokine storm) causing organ damage.
Those who are at a major risk for COVID-19 have known comorbidities including obesity, diabetes, asthma, autoimmune disease, hypertension, cancer, and chronic kidney disease which is the most prominent comorbidity leading to death.
These are the known health issues that can be dangerous for those who get infected with this coronavirus.
What about those of you who don’t know you have an internal health issue because you have had sub-standard and non-specific physical exams?!
COVID-19 has plagued the world since it was first identified in December of 2019. Many people who were infected with SARS-CoV2 recovered quickly and were able to resume their normal lives. But for some—and perhaps you—the effects of this viral infection can last for weeks and even months.
This phenomenon is called “long Covid,” and if you suffer from symptoms post SARS-CoV-2 infection, you are now considered a “Long Hauler.”
During the initial infection with the coronavirus, symptoms can range from fever, chills, and muscle pain to fatigue, headaches, sore throat, shortness of breath, and a loss of taste or smell. Other symptoms can include—chills, chest pain, nausea, vomiting, diarrhea, and skin rashes.
The Cytokine Storm and hyperinflammation
As your body’s immune system neutralizes the virus, both the innate and adaptive immune responses are actively killing cells infected by the virus and producing antibodies. During this battle, white blood cells release cytokines—chemical messengers that recruit and regulate different types of white blood cells to help fight in the battle.
While it’s normal for white blood cells to releases cytokines during a coronavirus infection—in genetically susceptible people—white blood cells can release too many cytokines creating a pro-inflammatory state called a “cytokine storm.”
Data out of Frontiers in Immunology, reports this uncontrolled systemic inflammatory response can cause, splenomegaly (enlarged spleen), hepatomegaly (enlarged liver), lymphadenopathy (swollen lymph nodes), clotting disorders, dysfunction in the nervous system, and ultimately multiple organ damage and/or failure.
This hyperinflammation can cause many different symptoms including flu-like symptoms, fatigue, swelling of your limbs, joint pain, shortness of breath, rapid breathing, seizures, tremors, confusion, hallucinations, low blood pressure, and lethargy.
What about those who don’t develop hyperinflammation and serious lung and organ damage?
Long covid symptoms can exist for weeks and months after the acute SARS-CoV-2 infection
After the acute immune response cools off and the immediate coronavirus infection is not a serious health threat, many people are now exhibiting post-acute covid-19 of “long covid” symptoms weeks and months after the acute COVID-19 infection. In some cases, new symptoms develop and evolve long after the initial viral infection.
If you are a long hauler, you may experience periods of symptomatic improvements followed by those same symptoms getting worse again. If you suffer from “long-covid” you may have some or all of these viral-persistent symptoms:
-
-
- *Post-viral fatigue and a lack of energy
- Respiratory issues – shortness of breath or difficulty breathing, and chronic cough
- Neurological dysfunction—dizziness, brain fog, neuropathy, a loss of smell and taste, sleep issues, poor concentration and memory problems
- Cardiovascular complications—inflammation of the heart muscle, palpitations
- Dermatologic/skin issues—rash, hair loss
- Hepatic dysfunction—elevated liver enzymes
- Digestive issues—disruption of nutrient absorption, abdominal pain, gastritis, diarrhea.
- Emotional symptoms—depression, anxiety, and mood changes.
- Immune dysfunction—flare-up of autoimmune disease, autoinflammatory diseases, and chronic inflammation
- Chronic pain—joint and muscle pain
-
A small study posted in the Journal of the American Medical Association found 87.4% of people who recovered from COVID-19 had persistent symptoms. [Image from the Journal of the American Medical Association]
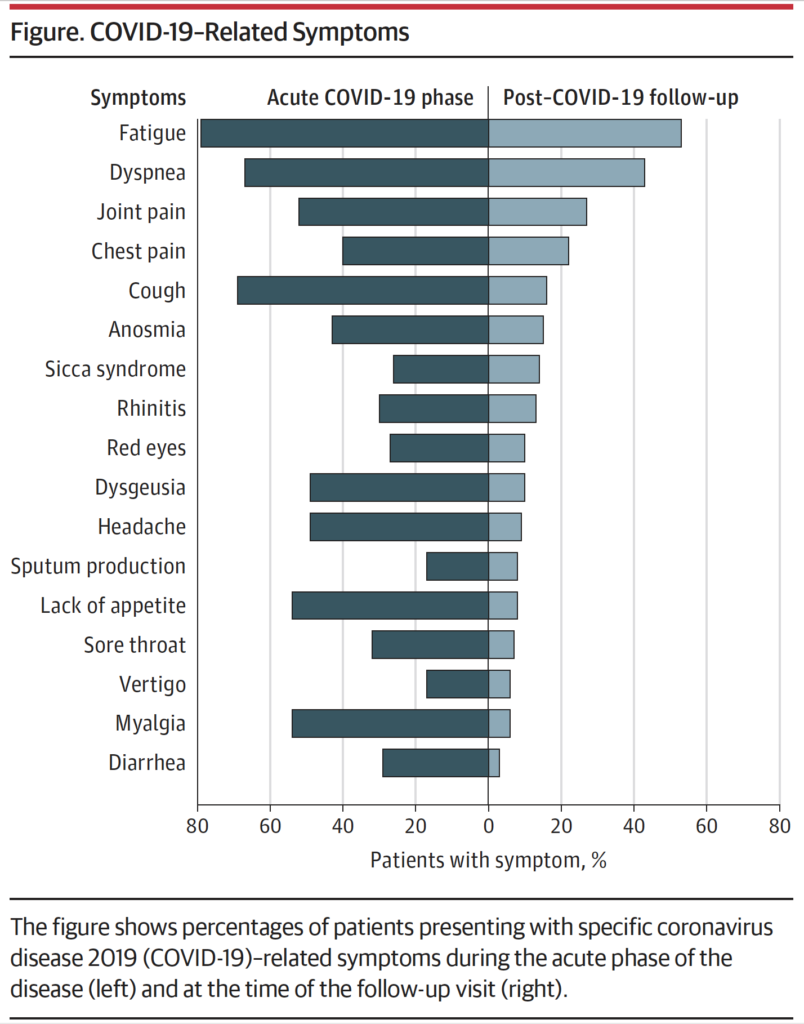
The lack of symptom history created this study’s limitation. However, the individuals in this study had persistent symptoms that many people outside of the study experience.
Health “authorities” are talking about it; no one knows how to rebuild from it—the long-term dysfunctions and symptoms following a SARS-CoV-2 infection.
Whether you suffer from crippling fatigue, shortness of breath, or joint pain, “long covid” seems to be a multisystem disease that needs a functional approach to improving physiology and eliminating symptoms.
What’s causing your post-covid symptoms?
During a SARS-CoV-2 infection, the immune system not only fights the infection, specific white blood cells get injured. Data from the American Society for Microbiology, reveals white blood cells get injured from SARS-CoV-2, while other white blood cells develop a memory of this viral infection.
Injured white blood cells and cells that have a memory can result in an imbalanced and broken immune response which can lead to chronic inflammation and an inability to heal through viral infections including this coronavirus.
Data also point to dysfunction within the cell’s energy-producing organelle, the mitochondria. Do you remember the body’s energy source adenosine triphosphate (ATP)? Mitochondria are also needed for proper immune function and the maintenance of normal cellular functions.
When cells and their mitochondria are under stress, the cells turn on specific pathways for recovery to bring back cellular homeostasis. However viral infections are associated with altered cellular physiology.
Research out of the journal Mitochondrion, states mitochondria are highly prone to various cellular stressors that can damage the mitochondria—one being viral infections. Damaged mitochondria cease to produce energy, support our inherent immune response and cease to maintain normal cellular functions.
According to the American Journal of Physiology-Cell Physiology, the powerhouse of the cell—the mitochondria—produce proteins called mitochondrial antiviral signaling proteins which serve to induce cell suicide when the cell is infected with viruses. The researchers also describe the hijacking of the cell’s mitochondria by SARS-CoV-2 for its advantage.
Basically, the virus can alter the function of mitochondria preventing the cell from committing suicide ultimately leading to more viral particles being made.
This manipulation by the coronavirus can increase inflammation and suppress our innate and adaptive immunity.
Could the reason long haulers suffer from debilitating fatigue and the long list of other symptoms be due to an injured immune response and dysfunctional mitochondria caused by SARS-CoV-2?
But wait, there’s more.
In order to transfer the energy from the foods we eat to normal cellular functions, we need nicotinamide adenine dinucleotide (NAD+). As we age, we develop decreased energy, increased fatigue, and perhaps a loss of motivation.
With age, we also have fewer NAD+. Less NAD+ leads to impaired mitochondrial function which is associated with many of the physical symptoms of aging. NAD+ is needed to take food energy and transfer it into the mitochondria where ATP is produced.
A loss of NAD+ is also seen with the coronavirus infection. Researchers out of the School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran, found the SARS-CoV-2 virus not only caused damage to the cell’s DNA, but it also led to the depletion of NAD+ and ATP which ultimately caused cellular death.
So, the SARS-CoV-2 virus can damage the immune system, enable it to create inflammation and the virus can deplete NAD+ and damage mitochondria with a reduced level of ATP production preventing cells from creating energy for normal cellular function.
This sounds like post-viral fatigue.
Rebuild from Long-Covid
While data continues to emerge regarding the long-term effects of the SARS-CoV-2 infection, it makes sense to take a functional approach to rebuild the internal terrain of the body following infections from SARS-CoV-2. This means taking the appropriate actions to restore and rebuild the immune response, support and rebuild mitochondria, and reduce chronic inflammation.
Rebuild proper immune function.
Notice how I didn’t say “super-charge” or “enhance” your immune response. Why? According to research out of MedRXiV long-after someone tests negative for infection, immune cells can create persistent systemic inflammation.
The point is, if you are a long hauler you want to normalize and rebuild the immune response, so it doesn’t become more aggressive. You don’t want to activate an already primed immune system.
To normalize immune function and get rid of damaged and programmed white blood cells, immune cell recycling—autophagy (aww-toph-a-gee)—is recommended. When cells are damaged or parts of the cell is damaged, the cell recycles itself. By doing so, new immune cells can be produced with their inherent normal functions.
Activating immune cell autophagy can be done with calorie restriction. Calorie restriction is reducing your daily caloric intake by 30-50%. Caloric restriction has been shown to activate genes the produce sirtuin proteins that regulate gene expression and cellular renewal.
You may be familiar with the concept of fasting.
Fasting physiology involves reducing caloric intact for short periods of time. However, calorie restriction does not mean nutrient restriction. Nutrients are needed to run biological systems and restore function. In fact, nutrient deprivation is dangerous.
Eliminate gluten, dairy, and white refined sugars, and starches. Focus on eating nutrient-dense foods, good fats high in omega-3 fatty acids, and foods containing polyphenol and flavonoids—rainbow colored fruits and veggies.
Consider eating insoluble fibers (cauliflower, peas, prunes, dark leafy vegetables, blackberries) and fermented foods (pickles, sauerkraut, kimchi) to support normal gut function and restore normal gut flora. There is evidence that your gut health and the different species of bacteria in the gut can help immune cell recycling.
Nutrients that support normal immune function include vitamin A, vitamin C, vitamin D, zinc, omega-3 fatty acids, beta-glucans from mushrooms, and probiotics.
Rebuild proper mitochondrial function and energy production
Mitophagy is autophagy for the mitochondria. Again, calorie restriction is a simple action to take to restore mitochondrial function and activate mitophagy.
Increased mitophagy can be created by taking Coenzyme Q10. You may be familiar with CoQ10 for those using cholesterol-lowering drugs (statins). CoQ10 is not only needed to preserve heart function while taking statins and chemotherapy drugs but also to rescue your mitochondria.
CoQ10 is the most important antioxidant our cells need to support and protect mitochondria. Without CoQ10, the level of ATP that the mitochondria produce drops, and the energy for cellular function decreases.
Having normal mitochondrial function is synonymous with healthy NAD+ levels and ATP production.
To produce NAD+ you need vitamin B3—niacin. Niacin can be used to synthesize NAD+ through a specific pathway called the salvage pathway. NAD+ is also produced by the consumption of the amino acid L-tryptophan.
Do you recall Thanksgiving turkey and tryptophan? Dietary tryptophan is a primary source of NAD+ needed for proper immune function.
Controlling chronic inflammation
Since SARS-CoV-2 has been in the limelight, hyperinflammation is the acute cause of damage and now chronic lingering inflammation is causing the long-term symptoms associated with the virus—a.k.a long covid.
Cytokines are immune messengers that communicate with different cells of the immune system. When the immune system becomes overactive during a cytokine storm, the prominent cytokine in charge is interleukin 6 (IL-6). IL-6 is implicated in acute respiratory distress syndrome causing lung damage and is involved in multi-organ failure for those with severe infection and COVID-19.
White blood cells contain a genetic switch called NF-kB. NF-kB is the orchestrator of inflammation and responsible for the production of IL-6. Under times of acute or chronic inflammation, white blood cells produce IL-6 which travels into the liver where C-reactive protein (CRP) is created. You may be familiar with CRP when getting your physical exam and blood work.
By far the greatest regulator of NF-kB and one of the most powerful anti-inflammatories is curcumin. In fact, data out of Immunopharmacology and Immunology, reveals curcumin to be a powerful inhibitor of NF-kB and IL-6.
Additional nutrients that inhibit NF-kB include fish oils, lipoic acid, and N-acetyl cysteine, reishi mushrooms, and epigallocatechin gallate (EGCG) found in green tea.
Summary
Collective data suggests there are multiple systems involved in long covid. As more and more research comes out, it would appear the known dysfunctions associated with being a long hauler is immune injury, mitochondrial dysfunction, and chronic inflammation.
The data also suggests—for now— rebuilding the internal terrain of the body after infection includes alterations in the diet and the use of specific nutraceuticals (supplements). It would also make sense as your fatigue improves to incorporate exercise back into your lifestyle as calorie restriction with exercise is an excellent and proven way to activate autophagy needed to clean up post-covid damage.
For more information on rebuilding from COVID-19, reducing chronic inflammation, or restoring your health after disease, get yourself a copy of Rebuild here or from your favorite retailer.


Recent Comments